
The old expression “April showers bring May flowers” is meant to celebrate the coming of spring, but for the millions of people across the US living with asthma, it’s more like a warning.
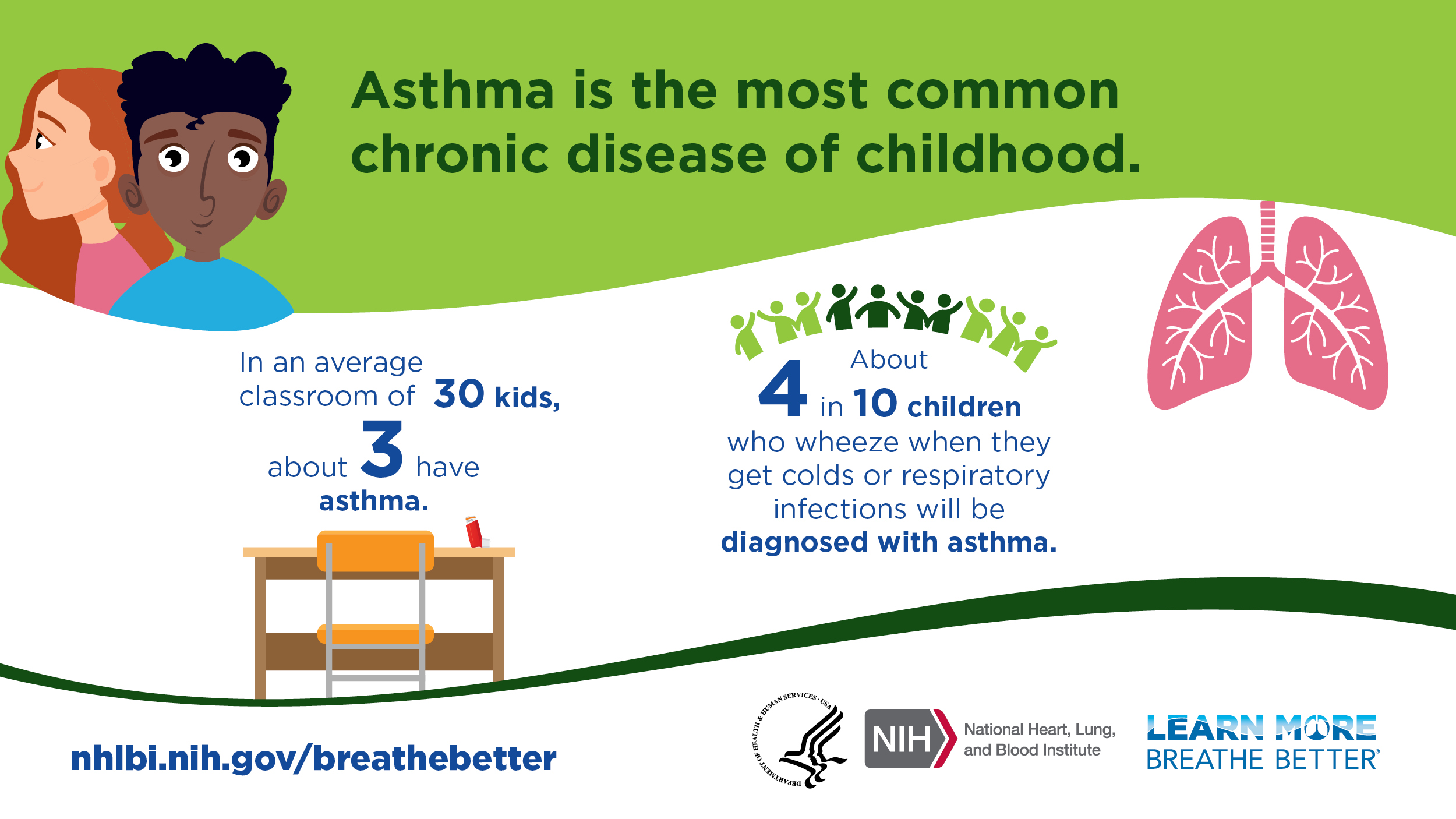
According to the Centers for Disease Control and Prevention (CDC), over 25 million people in the US have asthma. It’s also a leading chronic disease in young people, with more than 4 million children under the age of 18 diagnosed with asthma.
May is an important time of year in the fight against asthma, hosting events such as World Asthma Day and Air Quality Awareness Week as a part of Asthma Awareness Month. The purpose of these awareness campaigns is to promote better understanding of the disease for those who have asthma or know someone who does. They also serve as a reminder that the most effective way to manage asthma is to know and avoid your triggers and follow your doctor’s orders.
But what if you didn’t know you had asthma?
In this article, we’ll provide expert advice addressing common misconceptions about asthma, symptoms to look out for, and what you should do if you suspect you or a loved one may have asthma.
What is Asthma?
Asthma is a chronic lung disease that causes inflammation and narrowing of the airways, making it difficult to breathe. This condition affects people of all ages and often starts during childhood.
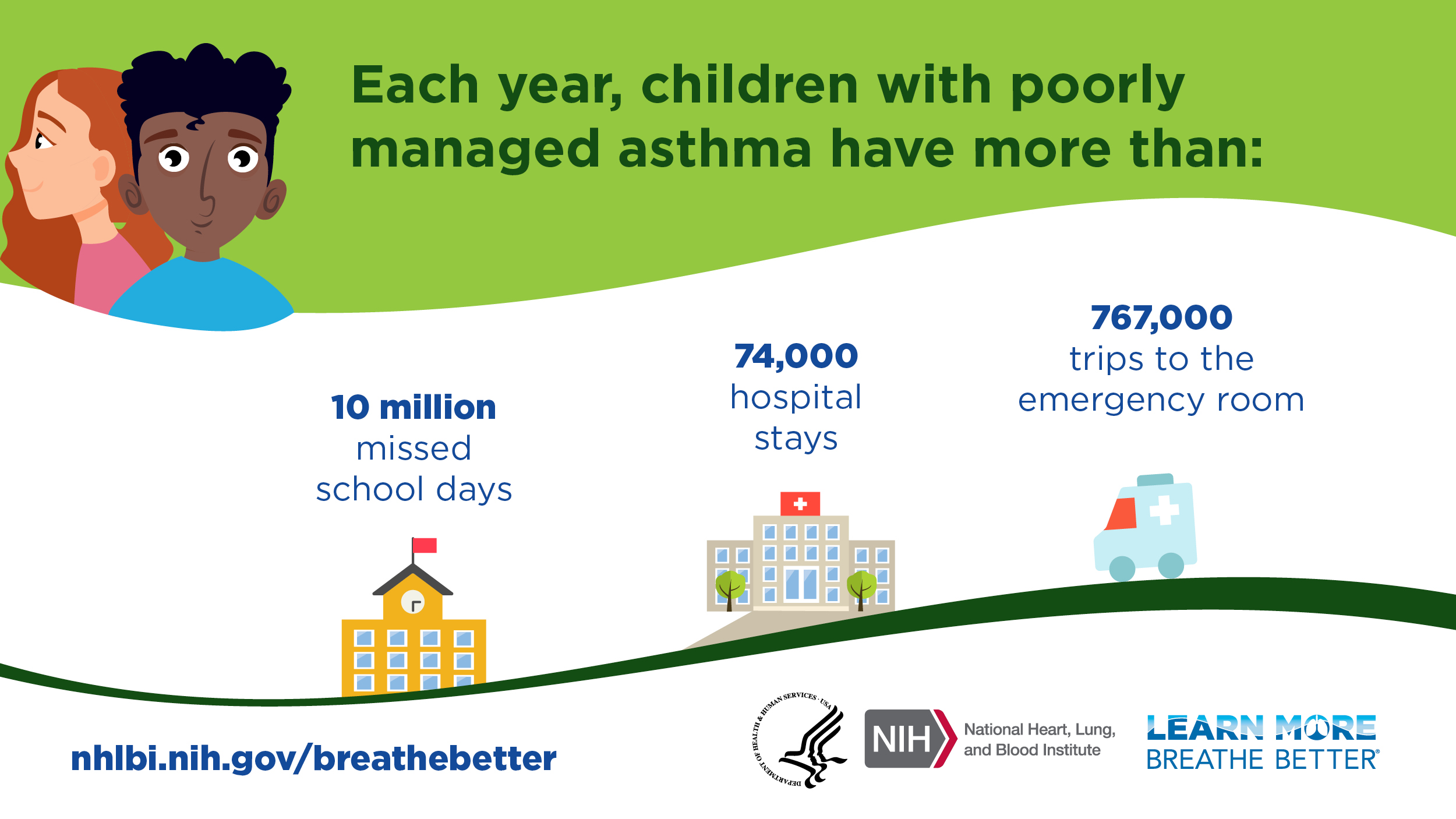
When inflammation occurs and airways begin to constrict, this is called an asthma attack. These attacks can be dangerous and potentially life-threatening—according to the National Heart, Lung, and Blood Institute (NHLBI), asthma attacks lead to more than 1.6 million emergency department visits and 170,000 hospital stays each year.
Airway inflammation is caused by certain stimuli called triggers. These triggers can vary from person to person, and they can cause specific types of asthma symptoms to worsen depending on the amount of exposure and the severity of inflammation they cause. Some common asthma triggers include tobacco smoke, dust mites, air pollution, respiratory infections like the flu or COVID-19, and intense physical activity.
“When it comes to asthma, airway inflammation is the root of all evil,” said Dr. Lisa de Ybarrondo, a board-certified pediatrician and associate professor in the Department of Pediatrics at McGovern Medical School at UTHealth Houston in Houston, Texas. “It’s important to control your asthma and avoid your triggers because if you don’t effectively prevent and treat the inflammation, your symptoms are likely to get worse.”
Dr. de Ybarrondo is dedicated to the education and management of asthma. In addition to running an asthma clinic in the 1990s, she has been a faculty champion for NEEF since 2007 and has played a key role in teaching health care providers the foundational information and skills needed to care for pediatric patients with asthma.
Common Symptoms of Asthma
Not all people with asthma experience the same asthma symptoms, and the frequency and severity of symptoms can also vary from person to person.
“Your symptoms can be variable depending on the severity of the airway inflammation," said Dr. de Ybarrondo. “It’s possible you may not have what people consider a serious exacerbation because of a chronic, low-level of inflammation—not causing significant significant respiratory symptoms other than a cough that goes on for a long period of time.”
The following are some common asthma symptoms:
- Shortness of breath
- Cough
- Chest tightness or pain
- Wheezing (a whistling sound when breathing)
- Waking at night due to asthma symptoms
- A drop in your peak flow meter reading (if you use one)
Environmental Triggers for Asthma
Environmental triggers are a subset of asthma triggers that people come across in their daily lives—at work or school, at home, and in their neighborhood. Factors like climate change have led to increased levels of outdoor triggers such as pollen, ground-level ozone, and wildfire smoke. Several studies have linked the prevalence of asthma attacks and emergency room visits to an increasing number of summer days with high levels of air pollution.
While it's recommended for people with asthma to stay indoors on days with poor air quality, it's important to be aware of various indoor environmental triggers that can worsen asthma symptoms, including mold, pests, pet dander, and nitrogen dioxide from gas-burning appliances like stoves or fireplaces.
“Kids spend the majority of their time at home or in school, so it’s important to really concentrate on indoor triggers,” said Dr. de Ybarrondo.
- For more than a decade, NEEF has developed resources like this one to equip pediatric healthcare providers and clinicians with the knowledge and tools necessary to help their patients manage their environmental asthma triggers effectively.
- If you found this or any of our guides useful, please consider supporting NEEF with a one-time donation in honor of Asthma Awareness Month. Together, we can transform lives and create a world where everyone can breathe a little easier.
Who is Most At-Risk for Asthma?
While we still don’t know all the factors that lead to asthma, we do know that a person’s genetic makeup, local environment, and even where they work can contribute to developing asthma.
According to the Asthma & Allergy Foundation of America (AAFA), asthma is most common in male children and female adults. Like many chronic health conditions, the effects of asthma are not felt equitably. Asthma rates in the US are highest among Black adults, and non-Hispanic Black children are more than two times more likely to have asthma compared to non-Hispanic white children.
In 2020, the AAFA released a report highlighting the disparities in occurrences of asthma in the US. Compared to white Americans, Black Americans are 1.5 times more likely to have asthma, five times more likely to visit the emergency room due to asthma, and three times more likely to die from complications from asthma. The AAFA concluded that social determinants and structural inequities such as systemic racism are the main drivers of this health disparity, with factors such as genetics and individual behaviors contributing less.
Common Misconceptions About Asthma
When asthma is kept under control, it’s possible to live a normal life with relatively few chronic symptoms. However, there is still a lot about asthma that the public—and even health care providers—don’t fully understand. These misconceptions can make it more difficult to properly diagnose asthma and develop an asthma action plan, which is essential for managing asthma effectively.
We asked Dr. de Ybarrondo to help set the record straight on some common misconceptions about asthma.
Asthma Myth #1: You Can “Grow Out” of Asthma
Currently, there is no cure for asthma—once you are diagnosed, you have it for life. However, it is possible that your asthma triggers may no longer cause the same symptoms they once did, or even any noticeable symptoms at all. This can lead people to think their asthma is cured.
“One of the most common misconceptions I run across is parents thinking their kids will ‘grow out’ of their asthma,” said Dr. de Ybarrondo. She told the story of a former colleague with a history of reactive airway disease as a child who was in remission for many years, until a severe case of RSV (respiratory syncytial virus) caused his asthma to return with more persistent symptoms.
“Like with cancer, asthma can go into remission, but it can come back at any time,” she said.
Asthma Myth #2: You Need a Family History of Asthma
According to the American Lung Association, people with parents who have asthma are three to six times more likely to develop asthma than someone without a family history of the disease.
However, just as it’s possible to be genetically predisposed to asthma and not have it, it’s also possible to develop asthma in other ways, such as smoking, obesity, and exposure to certain asthmagens at work such as industrial and wood dusts, chemical fumes, molds, vehicle exhaust, and other unsafe air conditions.
It’s also just as likely that you may have a family history of asthma, you just don’t know it. Dr. de Ybarrondo said she often sees patients with asthma who have been misdiagnosed with some other condition.
“Some patients will say, ‘Oh, my doctor says I have chronic bronchitis,’ yet they have an inhaler and some of them actually have a controller medication, too,” she said.
Dr. de Ybarrondo believes these misdiagnoses could be caused by many different factors, including a stigma associated with asthma and those who have it.
“I think there is definitely a stigma in giving the diagnosis of asthma, because most parents know that asthma is a chronic lung disease, so they want to think of their child’s wheezing as being caused by something else,” she said.
Asthma Myth #3: People with Asthma Can’t Be Active
Asthma is much more common among athletes than you might think. According to the Allergy & Asthma Network, about one in 10 people have exercise-induced asthma (EIA), with symptoms that occur around 5-10 minutes after physical activity begins or ends.
In fact, a study conducted by the British Journal of Sports Medicine found that asthma is the most common chronic medical condition among Olympic athletes, especially swimmers, where the warm, moist air helps keep airway inflammation in check.
Regular exercise has many benefits for people with asthma, including improving lung function, promoting blood flow to the heart and lungs, weight loss, stress reduction, and a more resilient immune system.
Asthma Myth #4: Asthma Isn’t Life-Threatening
While deaths due to asthma are rare, especially among children and young adults, it is possible when symptoms are particularly severe. In 2020, the CDC reported over 4,000 asthma-related deaths, with adult females totaling approximately 60 percent of deaths that year.
The presence of certain health conditions, called comorbidities, can lead to more severe and life-threatening asthma symptoms. Common asthma comorbidities include obesity, obstructive sleep apnea, gastroesophageal reflux disease (GERD), and rhinitis/sinusitis.
The good news is that in most cases, asthma-related deaths can be prevented with early diagnosis, a consistent treatment plan, and access to quality health care.
The Environmental History Form on NEEF’s website is something I show to all the students, residents, nurses, and faculty that I teach,” said Dr. de Ybarrondo. “It’s a really great tool to help identify potential triggers.
Dr. de Ybarrondo
What You Can Do About Asthma
If you are concerned that you or your child may have asthma, you’re not alone. Millions of Americans with asthma are living healthy, active lives thanks to proper management of their asthma symptoms.
Speak with Your Health Care Provider
Your first step on your journey to managing asthma is to see a health care provider. They will ask questions to gather a full medical history and list of current symptoms. They will also conduct a physical exam and a spirometry test to measure lung function.
If your child does not have a primary care doctor, Dr. de Ybarrondo recommends talking to the school nurse—they are often the most qualified health care professional available to many families without health insurance.
“School nurses will often identify the kids who have more persistent symptoms because those are the kids that show up in their office on a regular basis,” said Dr. de Ybarrondo.
School nurses can also reach out to the primary care physician directly with their concerns. In most cases, in order for a child with asthma to have medicine at school, their primary care provider must provide their contact information and written permission.
“I’ve done a lot of lectures for school nurses, and I always tell them, ‘You are the front line,’” she said.
Develop an Asthma Action Plan
Once you have identified the right health care provider for your needs, work with them to develop an asthma action plan. This will help you track medicines, monitor symptoms and changes, and understand when emergency care is necessary. In Dr. de Ybarrondo’s home state of Texas, all schools require an asthma action plan.
Ask About NEEF’s Environmental History Form
Dr. de Ybarrondo says it’s important to find a primary care provider who will take the time to gather your full health history, including any symptoms and exposure to potential triggers.
"The Environmental History Form on NEEF’s website is something I show to all the students, residents, nurses, and faculty that I teach,” said Dr. de Ybarrondo. “It’s a really great tool to help identify potential triggers."
The Centers for Disease Control and Prevention’s (CDC) National Asthma Control Program has also developed a tool, EXHALE, that health care providers and people with asthma can use to help reduce asthma-related hospitalizations, emergency department visits, and healthcare costs.
Stick to Your Asthma Treatment Plan
Asthma may be a lifelong condition, but it doesn’t have to impact your quality of life, so long as you know your triggers, avoid them, and stick to your asthma management plan. Ignoring the symptoms won’t make it go away, and a lack of obvious symptoms doesn’t mean it won’t come back.
“While it's not curable, we have great ways to manage the symptoms and reduce the risk of an asthma attack,” said Dr. de Ybarrondo. “That’s important for parents to know, because if you have a kid with moderate to severe persistent asthma and they stop their controller medications, then their asthma symptoms and inflammation will come right back again.”
